Revision/redo weight loss surgery
All surgical procedures for obesity, both old and new, are designed to change how the person processes food. Although all of these procedures are designed to be permanent, in reality not all the effects of the surgery are permanent. Over time, parts of the stomach and oesophagus can stretch and sag, and patients can develop new conditions such as ulcers or reflux. In general, these operations are like anything mechanical: the better you maintain it, the longer it lasts. Unfortunately it is very common for patients to drift away from their initial enthusiasm and gradually stop looking after themselves and their operation. This can lead to weight regain, problems with how the operation works, and complications that require surgical intervention. Unfortunately, being compliant and sensible does not guarantee a hassle – free operation, although it will reduce the risk of problems by about 75 per cent. Many of the older types of operation (stomach stapling, older banding operations) also had design faults that led to problems in their function over time, even if patients did the right thing.
In general, between about 10 and 30 per cent of patients having any type of weight loss surgery will end up needing later surgery to treat complications or weight regain. One of the main reasons patients should return to their surgeon for follow – up is to reduce the risk of repeat surgery, and to notice and treat any problems early.
Weight Loss Surgery Complications
Lap band
Patients who have their band inappropriately tight, who experience frequent vomiting or chest discomfort when they eat will usually end up with a slipped band or stretched stomach or oesophagus. The risk of this complication is about 5 – 15 per cent per year if the band over tight, and 1 – 2 per cent per year if the band is looked after appropriately. Patients with this complication will experience regurgitation, reflux and sometimes complete band blockage (slip). Complete band blockage can require emergency surgery if band deflation does not work. Less common band complications include band erosion or infection (0.25 per cent per year), and problems with the band port. Apart from acute band blockages, the large majority of band complications are easy to treat.
Gastric Sleeve
Acute infections after surgery are uncommon, but usually require corrective surgery. The most common complication after a sleeve is reflux, and in approximately 10 per cent of patients further surgery is needed later to help correct this (either hiatus hernia repair or gastric bypass are the most common procedure s)
Gastric Bypass Surgery (RYGBP)
Acute infections after surgery are uncommon, and some require surgery if they occur. About 1 in 20 patients require endoscopy (gastroscopy) in the first few months after surgery. The worst potential complication after gastric bypass is obstruction (blockage) of the small bowel; this occurs in 1 in 20 patients and usually presents as recurrent abdominal pain in the left upper part of the abdomen (with pain radiating to the back). Unfortunately, although the problem is very easy to fix for most people, delay in diagnosis because patients and their doctors ignore or misdiagnose the pain can lead to real problems. The most common cause of death after this type of surgery is due to delayed diagnosis or inappropriate treatment of obstruction of the small bowel.
Other potential complications from gastric bypass include ulcers (especially if patients drink alcohol or take aspirin – like drugs), and less common problems such as gastro – gastric fistula.
Surgery for weight regain
Revision surgery is quite common. To date We have performed about 500 re – operations on weight loss patients.
All weight loss operations suppress appetite and make the patient eat slowly. If the person learns to eat small, regular meals (three meals a day) and avoid snacking and liquid calories, they will generally do well in the long term.
For most patients with weight problems, the tendency to snack, graze and comfort eat was a major contributor to their original weight problem. If these behaviours persist after surgery we expect their weight problem to come back. Some weight regain occurs in the large majority of patients after surgery, usually due to snacking rather than to eating large meals.
Thankfully, many patients seek help when they start to regain weight, and can get back on track relatively easily, but there are others who only seek help after they have regained large amounts of weight. This group probably accounts for about 75 per cent of the patients who need redo surgery after a previous weight loss operation. They can be easily identified because they have previously stopped coming in for follow – up, they have stopped taking their vitamins and have recommenced bad lifestyle choices. In the other 25 per cent of patients requiring redo surgery, weight regain is due to the development of a technical problem with their operation. If they present before they have had massive weight gain, solving the problem is fairly straightforward.
Options for redo surgery
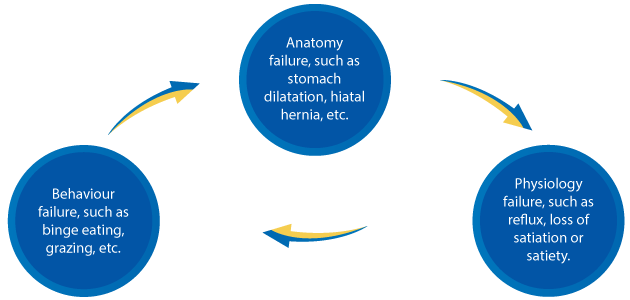
All patients with weight regain need:
- Assessment of the anatomy of their operation, in order to make sure that it is correct (this might involve barium x – ray, CT scan or endoscopy
- Assessment of their eating behaviour (binge eating, grazing, night eating disorder, alcohol, high energy snacks)
- assessment of the physiology or function of their operation (hunger, reflux, food capacity)
If a patient needs redo surgery we can then create a solution that is specific to your particular problem that a patient has. Redo surgery can be planned to
- Fix a complication with an operation
- Repair or fix an operation that is no longer working
- Change an operation to another procedure (band/sleeve/bypass)
In some circumstances it is preferable to reverse the original operation and decide on further treatments later on.
As the options above are so wide and varied, it is very important to take the time to find the right solution for each person as an individual.

